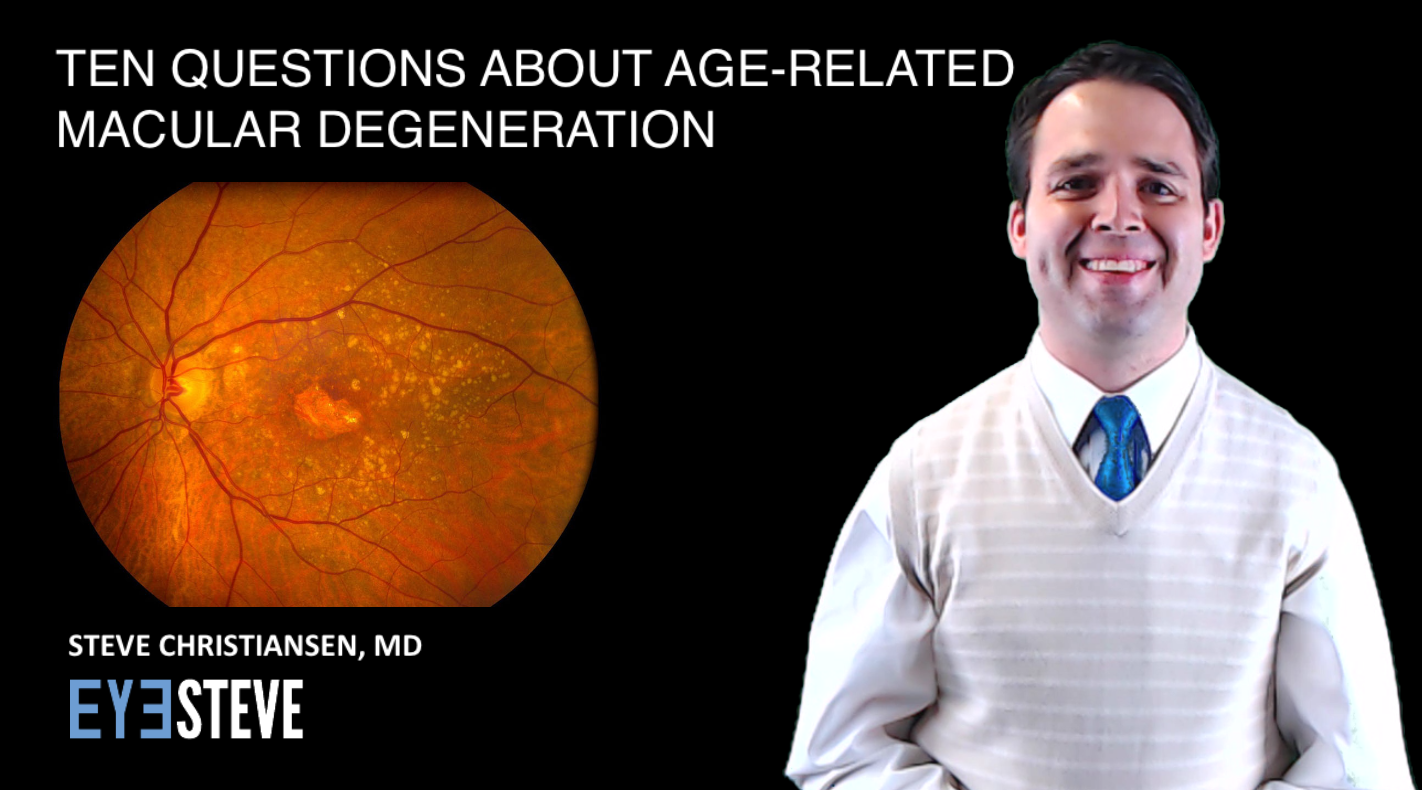
This month, February 2018, is age-related macular degeneration month. With the purpose of increasing awareness of this vision-limiting and life-altering disease, here are ten common questions about age-related macular degeneration.
Question #1 – What is macular degeneration?
Macular degeneration is a degenerative disease which causes damage to the macula, the part of the retina which gives us the clarity and fine-detail of our central vision. Our eyes are like a camera, and the retina is like the film in our cameras, as all the light from our surroundings is focused onto the retina. This information is then sent from our retina to our brain to be interpreted into what we see. The most important area of the retina, with the greatest concentration of light-sensing cells, is the macula, and in macular degeneration, these light-sensing cells become damaged. Macular degeneration is a generic term referring to various degenerative diseases of the macula, but in this video we will only discuss age-related macular degeneration, a leading cause of severe vision loss worldwide, especially among older, Caucasian individuals.
Question #2 – What are the symptoms of macular degeneration?
Because macular degeneration involves damage to the macula, which is the area of the retina that corresponds to our center vision, the symptoms of macular degeneration commonly involve one’s central vision. More specifically, patients with macular degeneration often complain of blurry central vision. You may notice this blurry central vision as difficulty reading, trouble recognizing faces from afar, trouble completing normal daily tasks or needing more and more light to complete daily tasks. You may also notice distortion or waviness to objects in your central vision, such as the side of a doorway or a street light. Several of these are also symptoms of cataracts or other conditions, so it is important to see your eye doctor if you notice changes in your central vision to determine the cause.
Question #3 – My doctor gave me a square grid and told me to look at it every day, what is this grid and how do I use it?
We often give patients with early or stable macular degeneration a grid. This is what is known as an Amsler grid, and could alert you and your doctor to changes that, if treated early, could help prevent or prolong vision loss from macular degeneration. To use this grid, simply close or cover one eye, and with your glasses on, if you wear them, hold the grid about a foot away, looking at the dot in the very center. While still maintaining focus on the center dot, check to ensure that all other lines in the grid appear straight, or in other words, be sure none of the other lines in the grid appear distorted or wavy. If things appear normal, uncover that eye, cover the other eye, and repeat the same process. If you do notice wavy or distorted lines in either eye, call your eye doctor right away.
Question #4 – I’ve heard there are two forms of macular degeneration, wet and dry, what does this mean?
Dry macular degeneration is the most common form of the disease, and if you had a room full of 100 individuals with macular degeneration, 85 or 90 would have dry macular degeneration, which typically involves slow, gradual damage to the light-sensing cells in the retina. The dry form of macular degeneration involves the accumulation of small, yellowish lipid-deposits called drusen. These deposits can be present even in normal individuals, and likely do not cause age-related macular degeneration, but having drusen increases a person’s risk of developing macular degeneration.
Wet macular degeneration may also include the presence of drusen, but wet macular degeneration specifically refers to the growth of an abnormal blood vessel from beneath the retina. This abnormal blood vessel, known as a choroidal neovascular membrane, then leaks fluid, often blood, into the layers beneath and within the retina. This fluid then damages the light-sensing cells of the macula. Fortunately, we have several treatment options to help control the growth of these abnormal blood vessels and the harmful fluid they leave behind.
Question #5 – Will I go blind from macular degeneration?
Macular degeneration, if very advanced, may severely limit your vision to the point of you being able to only count fingers or see hand movements in your central vision. This level of vision loss is considered legal blindness, and certainly may have a severe impact on daily life, but macular degeneration will not lead to complete and total blindness. Your peripheral vision will typically be preserved, but will unfortunately not provide the same crisp clarity because the still-healthy retina outside of the central macula does not have nearly the same density of light-sensing cells. In other words, age-related macular degeneration may lead to severe visual impairment, but will not cause you to become completely blind.
Question #6 – What is the treatment for dry macular degeneration?
Researchers are working vigorously to discover new treatments for dry macular degeneration, but there is currently no treatment to restore vision lost from the dry form of this disease. A very large study sponsored by the National Eye Institute (AREDS and AREDS2), determined that several minerals and anti-oxidants may prevent patients with an intermediate stage of dry macular degeneration from going on to develop advanced macular degeneration, both of the wet and the dry forms. These minerals and anti-oxidants can be purchased without a prescription as AREDS2 supplements which you will take by mouth every day. If you have macular degeneration, ask your doctor if he or she thinks you might benefit from taking these AREDS2-vitamin supplements.
Question #7 – What is the treatment for wet macular degeneration?
While we do not currently have great treatment options for dry macular degeneration, we have excellent options for the wet-form of the disease. Remember that the main characteristic of wet macular degeneration is the abnormal blood vessel growing from beneath the retina and leaking fluid which then damages the light-sensing cells of the retina. We fortunately have several options to help control the abnormal blood vessel growth and bleeding in wet macular degeneration. These medications are given directly into the eye by your ophthalmologist, and may be needed as frequently as every month to control the disease.
Question #8 – My grandmother or grandfather has age-related macular degeneration, will I get macular degeneration?
Both genetic and environmental factors have been found to be associated with the disease, but macular degeneration does not have a clear and well-established inheritance pattern, like many other diseases. It is estimated, however, that approximately 15 to 20 percent of individuals with age-related macular degeneration have at least one first-degree relative such as a sibling or parent, with the disease.
Question #9 – What can I do to prevent macular degeneration from developing?
Several risk-factors have been linked to macular degeneration and should be avoided, including smoking, obesity, high blood pressure, and diets high in fat, cholesterol. A diet rich in green, leafy vegetables and anti-oxidants may lower risk of the disease. And as was mentioned previously, the AREDS2 trial found that certain minerals and anti-oxidants may prevent the progression to advanced macular degeneration.
Question #10 – What vision-aids and other resources are available to those with advanced macular degeneration?
Individuals with advanced macular degeneration may have significant difficulty with normal tasks such as reading, paying bills, using a telephone, and other daily activities. Inasmuch as the central vision may be severely diminished, many options exist to help increase the projection of images from being focused on just the damaged area of the macula to being projected onto the areas of the retina that remain healthy and unaffected by the disease. This can be done via handheld magnifiers, digital magnification devices, phones with larger buttons, and various other features available on a smartphone or computer. Talk with your doctor if he/she might know of a low-vision specialist who may assist you with obtaining magnification devices and teaching you about the various accessibility features now available on your electronic devices.
I hope you have found this information about age-related macular degeneration to be helpful. Please share this information with your family, your friends, and your patients so that we may together increase awareness, screening, and, if necessary, treatment of this disease.







Great article! You have covered some important questions in the interview. Diabetes related macular degeneration has shown a pattern in being passed on to next generations in a family. If a person has genetic pre-dispositions to developing this disease, he/she should get routine eye-checkups from an age of 35-40.
Thanks so much for this article! My mother has wet AMD, as did 3 or possibly 4 of her siblings. I am doing all I can to prevent AMD. I eat a low fat, no added oil whole food diet of only plants (therefore no cholesterol), with a heavy emphasis on leafy greens. I have never smoked, I am thin and my blood pressure is very low. I keep an Amsler grid on the wall next to my desk. Thankfully, regular visits to the retina clinic at the University of Iowa show a perfectly normal macula with no sign of drusen – thank you God!
Sounds like you are doing everything you can! Great job and keep up the good work!