Accurately grading diabetic retinopathy can be a significant challenge for beginning ophthalmology residents. After nervously searching Google in the physicians workroom for the diabetic retinopathy grading scale more often than I care to admit, I have decided to summarize the classification criteria for diabetic retinopathy, at least in a way that makes sense to me. I hope you find this summary helpful.
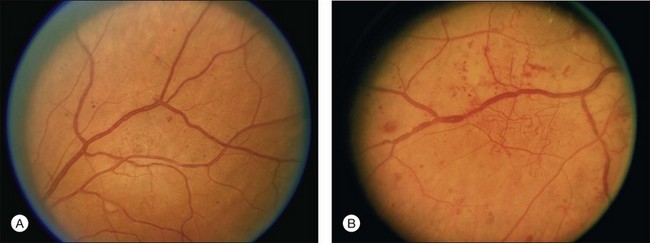
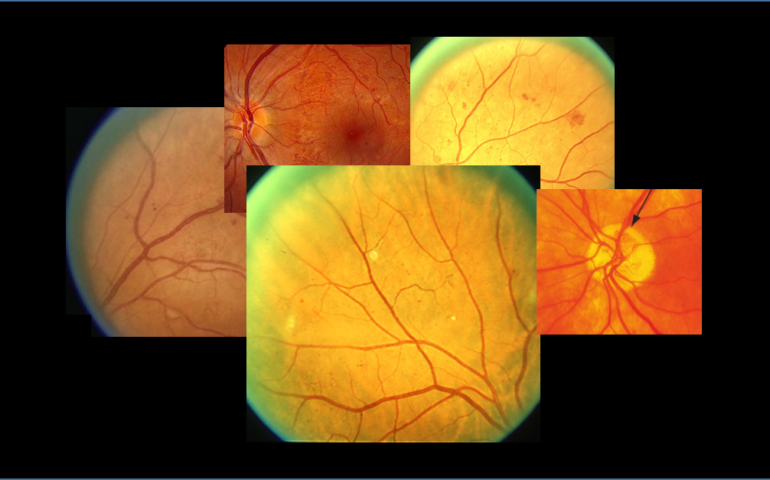
No retinopathy and mild NPDR
| Proposed Diabetic Retinopathy Severity Level | Exam Findings |
| No apparent diabetic retinopathy (No DR) | No abnormalities (no microaneurysms) |
| Mild nonproliferative diabetic retinopathy (Mild NPDR) | Microaneurysms ONLY |
In reality, there is not much difference in risk between diabetic eyes with no retinopathy and those with mild retinopathy. Both have a very low risk of progressing to PDR; in fact, the Early Treatment Diabetic Retinopathy Study (ETDRS) did not examine those with no retinopathy nor mild NPDR. However, the Wisconsin Epidemiological Study of Diabetic Retinopathy (WESDR) did include these individuals in its study, and found that the rate of progression to PDR after four years was less than 1% for both young and older patients with no diabetic retinopathy, compared to 4.1% in younger patients with a rare microaneurysm and hemorrhage and even less in older patients with these findings. In other words, a diabetic patient with no retinopathy has a <1% chance of developing PDR and a diabetic patient with a rare MA/DBH has a <5% chance of progressing to PDR in the next four years. All things considered, this is pretty low risk. These patients can be followed every 12 months.
Moderate NPDR
| Proposed Diabetic Retinopathy Severity Level | Exam Findings |
| Moderate nonproliferative diabetic retinopathy (Moderate NPDR) | More than just micro aneurysms (with or without cotton-wool spots, venous beading, or IRMA) but less than the 4:2:1 rule
More than “mild” but less than “severe” |
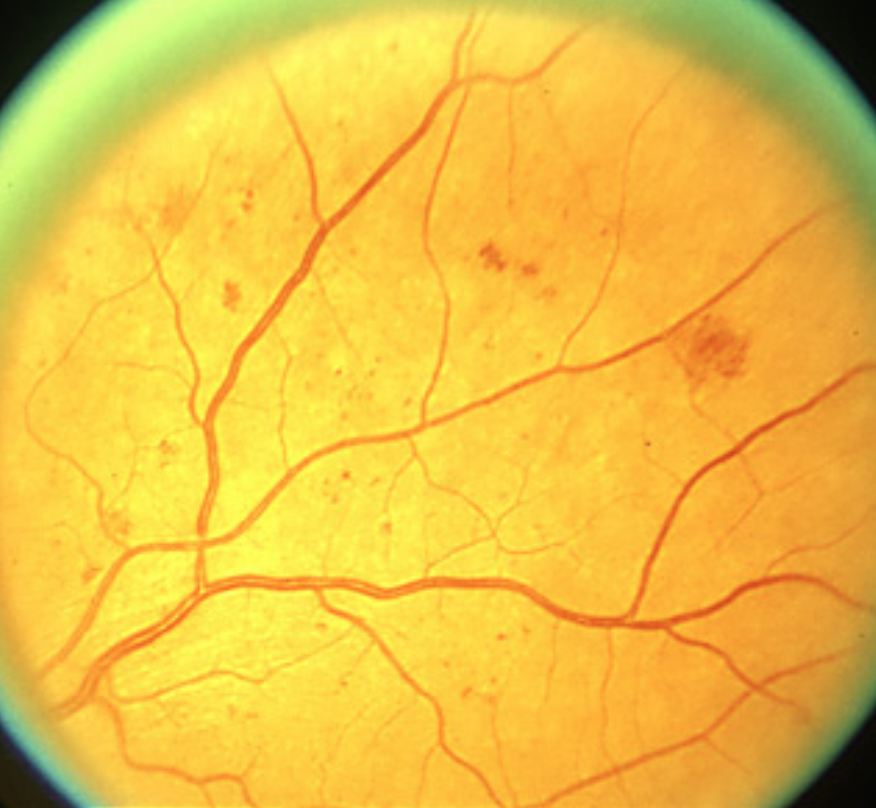
It helps me to simply remember that these eyes have more than just microaneurysms but less than any of the criteria in the 4:2:1 rule (described below). The WESDR stated that moderate NPDR contains dot blot hemorrhages (DBH) or microaneurysms (MA) as numerous and severe as the standard photo 2A below in at least one quadrant, with or without cotton wool spots (CWS), venous beading, or IRMA, but not achieving the 4:2:1 rule. This seems to be a fair number of patients I see in our VA Hospital retina clinic and are at a stage just before considering panretinal photocoagulation (PRP).
Severe NPDR
| Proposed Diabetic Retinopathy Severity Level | Exam Findings |
| Severe nonproliferative diabetic retinopathy (Severe NPDR) | Any of the following (4:2:1 rule):
· 20 or more intraretinal hemorrhages (dot blot hemorrhages) in each of all four quadrants · Definite venous beading in 2 or more quadrants · Prominent intraretinal microvascular abnormality (IRMA) in 1 or more quadrants |
Remember that the severe category is characterized by the 4-2-1 rule, and any eye meeting any one of the 4-2-1 criteria gets the distinction of severe NPDR. Patients with severe NPDR have a 17% chance of developing high-risk PDR within one year, and 40% chance of high-risk PDR within three years. These patients should be followed every 2-4 months, and may warrant consideration of PRP.
THE 4
The international clinical disease severity grading scale uses the general criteria of 20 or more intraretinal hemorrhages in each of the four quadrants, which is basically just a good way to think about how many hemorrhages it takes to have the quadrant you are examining be equal to the standard photograph 2A used in the ETDRS. The bottom line is this: if it looks similar to the photo 2A in one, two, or three quadrants, it is still moderate NPDR, but if it looks similar to photo 2A in all four quadrants, then the 4 of the 4:2:1 rule is satisfied, and it is severe NPDR.
THE 2
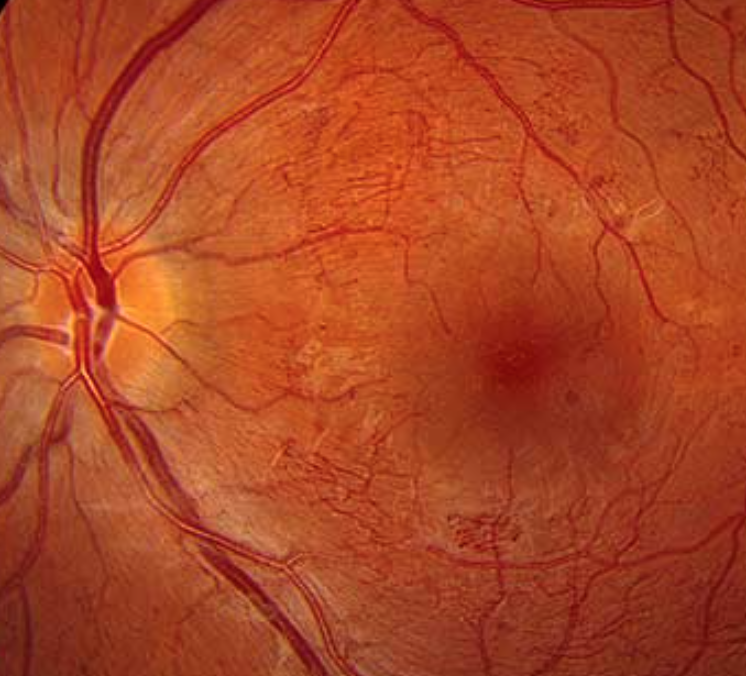
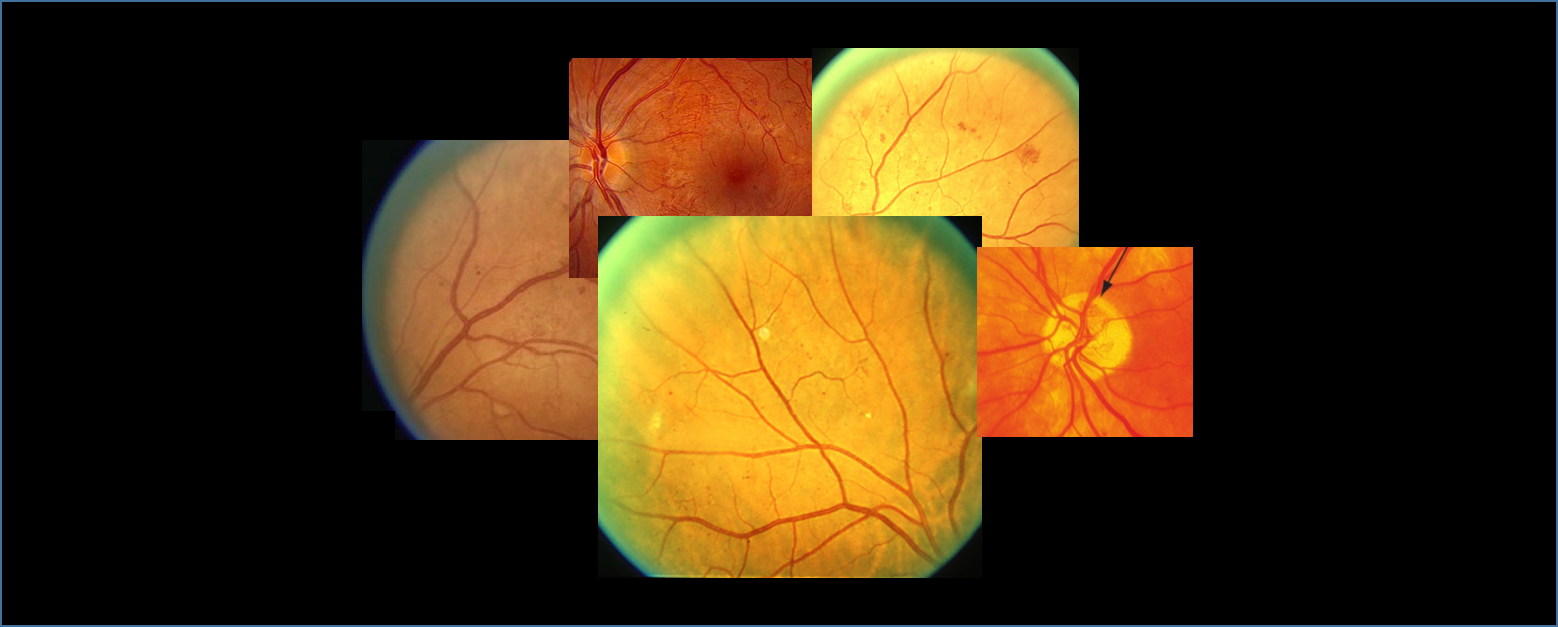
You may rarely (if ever) see severe venous beading to the extent of the ETDRS standard photograph 6B displayed below. Nonetheless, if you see a patient with this much venous beading in 2 quadrants, they have at least severe NPDR. It is thought that venous beading occurs when the walls of major retinal veins lose their normal parallel alignment and begin to appear like a string of sausages.
Standard photographs 6A and 6B, less and more severe standards for venous beading. ETDRS extension of the Modified Airlie House classification of diabetic retinopathy. (A) Less severe standard (6A). Two branches of the superior temporal venule show beading that is definite but not severe. (B) More severe standard (6B). Most large and small venule branches show severe beading. You should also note the presence of IRMA in both photos (discussed next).
THE 1
The presence of at least one IRMA in any one of the four quadrants automatically designates the eye as being severe NPDR and at high risk for progression. Photo 8A below is the standard photo used to describe an IRMA. Focus on the spidery-appearing vessels at the terminal branches of the venules. IRMAs are typically contorted in appearance with sharp corners. They typically do not cross over major veins or arteries, and may represent dilation of pre-existing capillaries. As stated below, IRMAs may even by slightly larger in caliber and more broad in arrangement than frank neovascularization. I have only seen one patient with a definite isolated IRMA in just one quadrant, which automatically placed him into the severe NPDR category. In my experience, IRMAs are either quite rare or just simply missed by most trainees, as they are not quite as easy to distinguish as MAs or DBHs. They appear similar to (and some argue they may even be) new, abnormal blood vessels growing within the retina (thus they are just one very small step from being deemed PDR).

Standard photo 8A showing the presence of intraretinal microvascular abnormalities. Also note the cotton wool spots.
Intraretinal microvascular abnormalities (or IrMAs) are shunt vessels and appear as abnormal branching or dilation of existing blood vessels (capillaries) within the retina that act to supply areas of non-perfusion in diabetic retinopathy. When compared to neovascularization (NV) in proliferative disease, IRMAs are slightly larger in caliber with a more broad arrangement and are always contained to the intraretinal layers.
Proliferative Diabetic Retinopathy (PDR)
| Proposed Diabetic Retinopathy Severity Level | Exam Findings |
| Proliferative diabetic retinopathy (PDR) | Either:
· Definite neovascularization OR: · Preretinal or vitreous hemorrhage |
The exact criteria for proliferative diabetic retinopathy can be very elusive to the beginning resident seeking to risk stratify the patient in front of them. Is the disc neovascularization covering 1/4 or 1/3 of the disk? Or is it 1/2 of the disc? What about neovascularization away from the disc? And is there vitreous hemorrhage? You may have the different criteria memorized but at this point, at least for me, it helps to simplify and think about PDR in very broad terms. As suggested in the AAO’s International Clinical Diabetic Retinopathy Disease Severity Scale, it comes down to this: Do they have disc neovascularization and/or vitreous/preretinal heme. If you can remember nothing else, that is all you need to remember. If there is NV and/or vit/pre-retinal heme, the patient has PDR. Another way to think about it is this: if they have vitreous (VH) or pre-retinal heme (PRH), chances are they have neovascularization either at the disc (NVD) or elsewhere (NVE), and alternatively, if they have NVD or NVE, they most likely also have VH/PRH or are prone to develop VH/PRH when the NVD/NVE bleeds. When you think about PDR in these broad terms, it makes it a bit less painful to try and risk stratify high risk PDR using the official DRS criteria, which are as follows (with my italicized comments to help you remember):
1. NVD ≥ 1/3 disc area: (your patient has more than 1/3 disc area of NVD? even if they do NOT have VH/PRH, that’s it, they have PDR, and you may have just missed the episode of the NV bleeding)
2. Any NVD with vitreous hemorrhage: (hey, they have NVD but also VH? Great! You caught the episode of the NV bleeding, making it easy to classify them as high risk PDR).
3. NVE ≥ ½ disc area WITH vitreous hemorrhage: (so they don’t have NVD but they DO have NVE of more than half a disc area AND VH? Just like #2 above, you caught the episode of that frond of NVE bleeding, so stratification is easy and they have high-risk PDR).
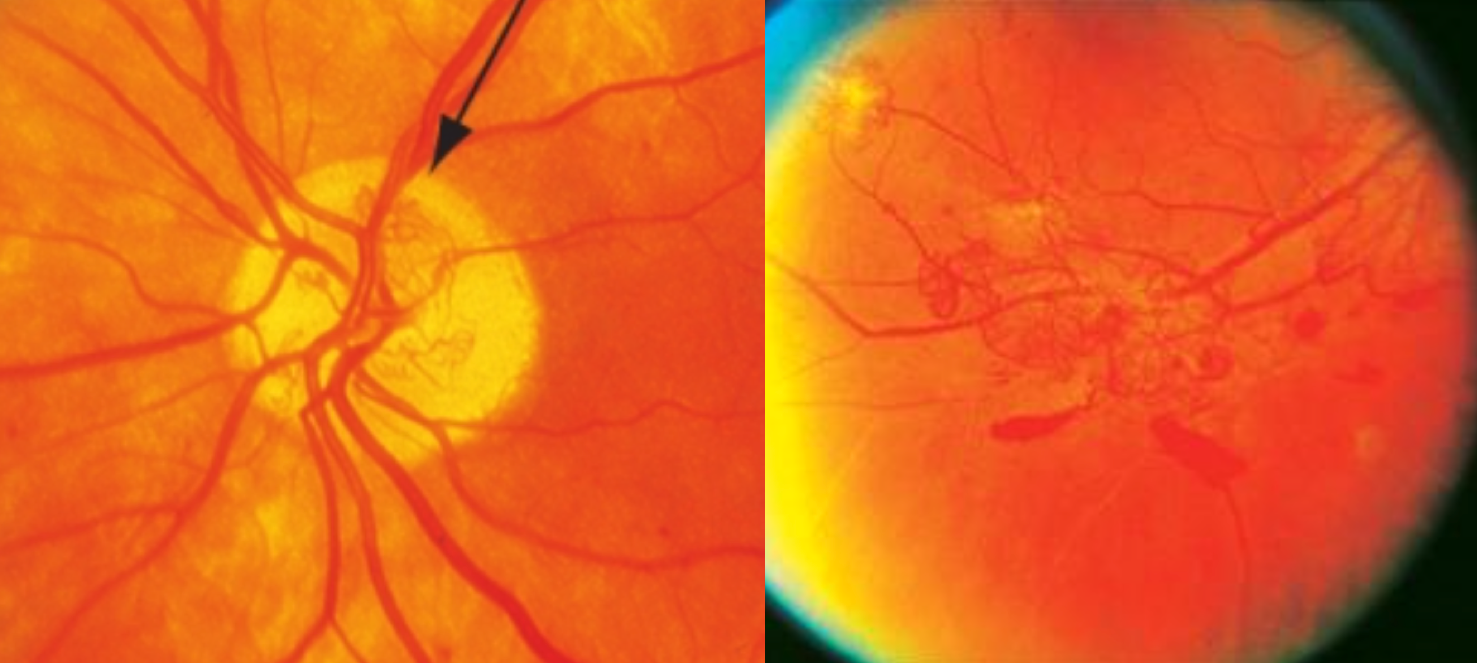
Standard photos 10A (left) and 7 (right) depicting approximately 1/3 disc area of NVD and at least 1/2 disc area of NVE, both of which would classify as PDR whether or not vitreous or pre-retinal heme was present.
High-risk PDR was also defined as three or more of the following high-risk characteristics (HRC’s):
1. Presence of vitreous hemorrhage or pre-retinal hemorrhage
2. Presence of any active neovascularization
3. Location of neovascularization on or within one disc diameter of the optic disc
4. NVD > 1/3 disc area or NVE > ½ disc area
Patients with high-risk PDR should receive scatter panretinal photocoagulation without delay. If they also have DME, you should either treat both simultaneously or treat the DME with focal laser first before doing PRP, as PRP can exacerbate macular edema. The anti-VEGF era, however, has changed this practice pattern, and many ophthalmologists now treat concomitant DME with PDR first with anti-VEGF (vs focal laser), particularly when the macular edema involved the central macula. If a patient has active PDR, they should be seen every 2-4 months. Once the PDR is no longer active or has involuted, they should still be seen every 6-12 months.
Diabetic Macular Edema
For any stage listed above, from mild NPDR to high-risk PDR, if the patient has macular edema, they should be seen every 2-4 months. The classification scheme for diabetic macular edema will be described separately.
And here is the entire table put together
| Proposed Diabetic Retinopathy Severity Level | Exam Findings |
| No apparent diabetic retinopathy (No DR) | No abnormalities (no MA’s) |
| Mild nonproliferative diabetic retinopathy (Mild NPDR) | Microaneurysms ONLY |
| Moderate nonproliferative diabetic retinopathy (Moderate NPDR) | More than just micro aneurysms with or without cotton-wool spots, venous beading, or IRMA but less than the 4:2:1 rule
More than “mild” but less than “severe” |
| Severe nonproliferative diabetic retinopathy (Severe NPDR); | Any of the following (4:2:1 rule):
· 20 or more intraretinal hemorrhages (dot blot hemorrhages) in each of all four quadrants · Definite venous beading in two or more quadrants · Prominent intraretinal microvascular abnormality (IRMA) in one or more quadrants |
| Proliferative diabetic retinopathy (PDR) | Either:
· Definite neovascularization OR: · Preretinal or vitreous hemorrhage |
If you would like more information, please visit these open-source links below
Link – A very nice summary by Brian Bucca, OD, FAAO at the University of Colorado describing the grading and classification of diabetic retinopathy in a similar format as this one, with very good descriptions of each standard photo and a bit more detail on the pathophysiology of each lesion.
Link – An open-source article in the World Journal of Diabetes on the diabetic retinopathy classifications.
Link – An AAO YOInfo article written by David W Parke III MD, “How to Classify the Diabetic Eye.”
Link – The Preferred Practice Pattern on Diabetic Retinopathy, written by the AAO and updated in 2016.
Links – While not open source, the ETDRS and WESDR both deserve recognition and links to their published articles
Link – From the AAO Preferred Practice Pattern above. Management Recommendations for Patients with Diabetes. This is the clinical practice guideline based on the classification of NPDR and PDR, as well as suggested interval for follow-up. Highly recommend checking this out and keeping readily available for reference in clinic.
Please let me know if this explanation helps you to better understand the classification of diabetic retinopathy!







excellent, informative but not elaborative, thank you
Excellent article ! Thank you.
Thanks. Keep writing, it eventually makes it clearer for us.