This is the first of a series of “Interesting Cases” posts (and videos) which I hope to publish here on EyeSteve.com. My goal with these videos is to, gradually, develop a library of short, concise videos which describe common (and even not-so-common) eye diseases using real-patient details and images, followed by a brief discussion of the disease and its most important features.
In this post (and video!), I will discuss branch retinal artery occlusions.
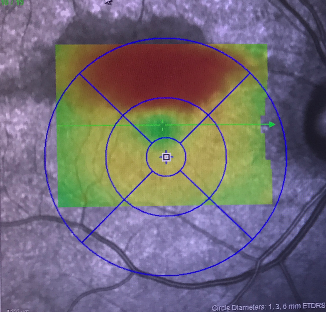
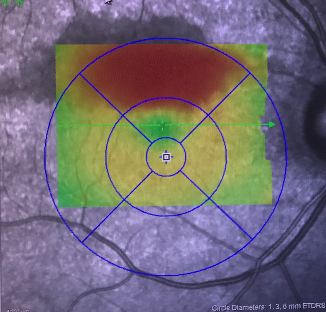
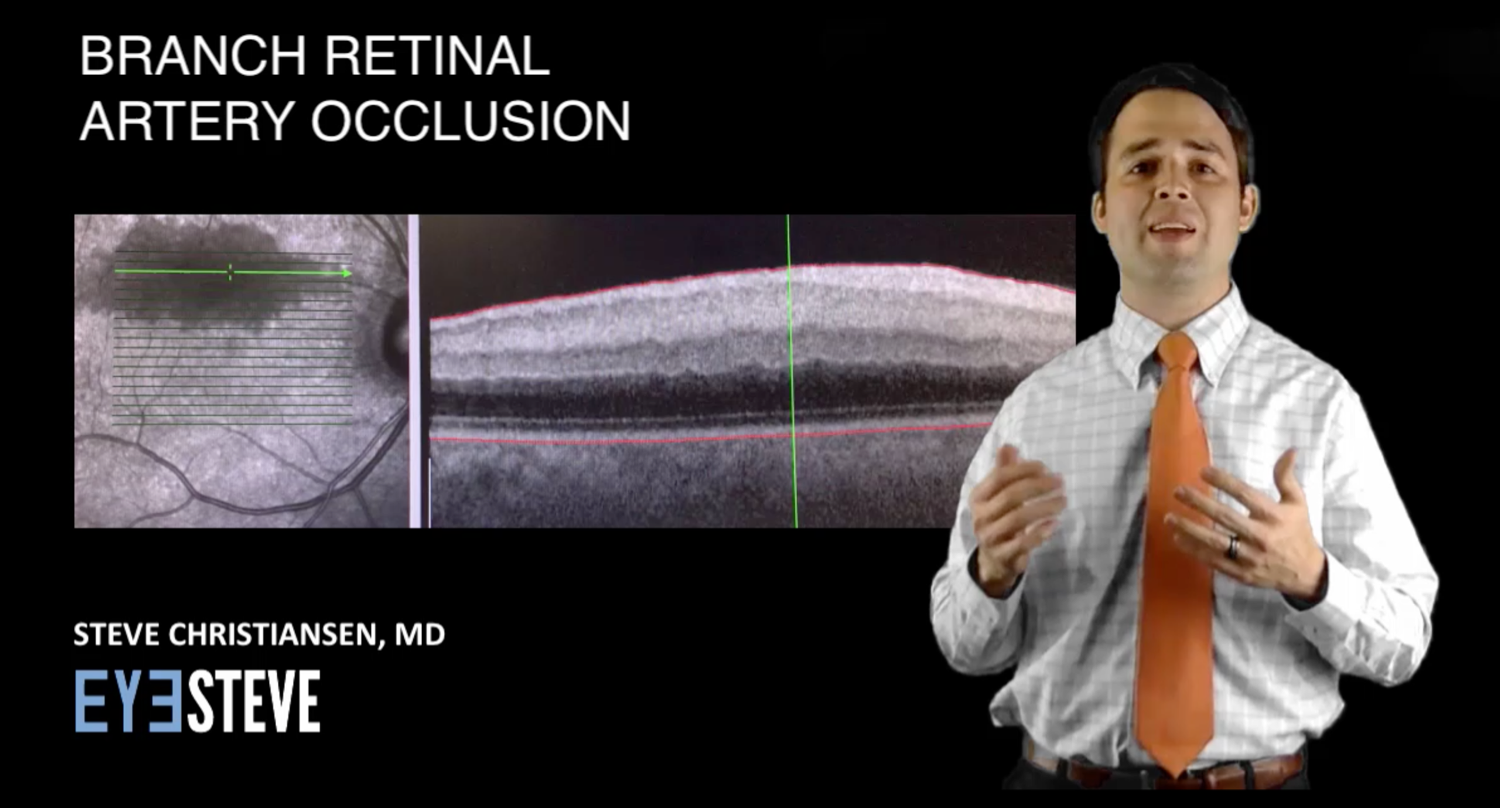
This is a fundus autofluorescence and macular thickness map of a 60 year old African American woman who complained of a black cloud in her inferior visual field which she noticed the prior day. She was hypertensive but had no other vascular risk factors. Her vision was 20/30 at this time. Here you can see hypoautofluorescence and thickening of the superior macula, suggestive of a branch retinal artery occlusion.
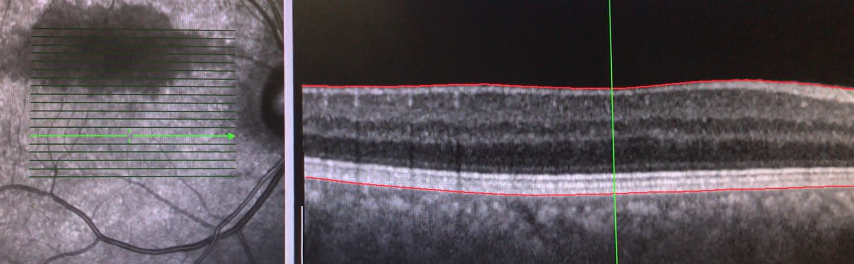
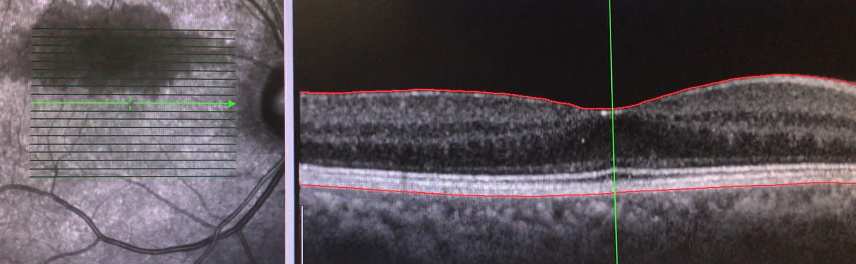
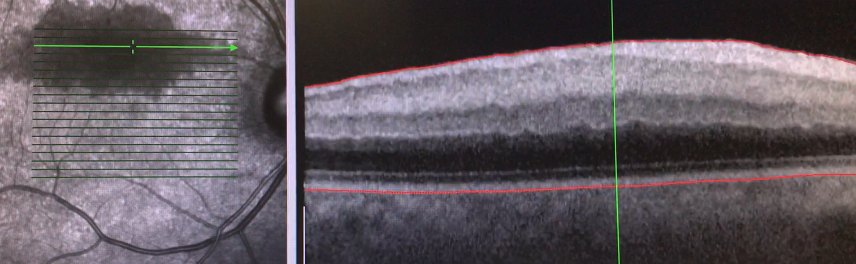
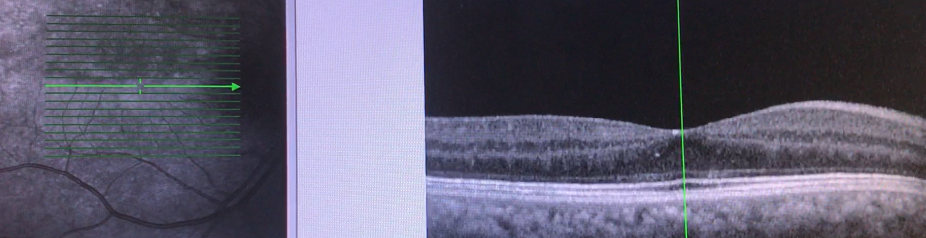
Here are several line scans through the macula. As you can see, the inferior macula is fairly normal, but the inner retinal layers show hyperreflectance and edema of the superior fovea and macula. Remember that the edema is isolated to the inner retina because this area is perfused by the central retinal artery and its branches.
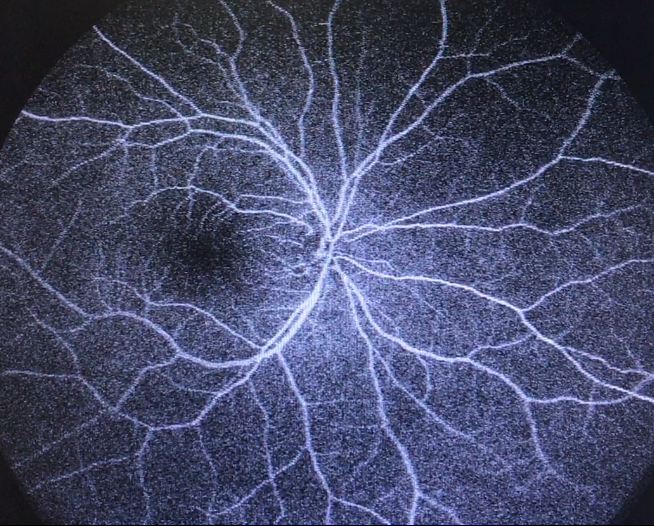
Interestingly, the fluorescein angiogram was essentially normal, without any visible arterial occlusion or area of non-perfusion, possibly because of only a short, transient episode of ischemia, which had already improved by the time she saw us.
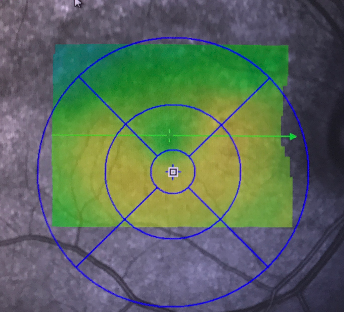
This OCT was taken about a month later, and shows the rapid improvement in the prior hypoautofluorescence and inner retinal thickening.
Here is a comparison of the thickness map between the two visits. Vision had improved at this time to 20/25 and she had noticed a lessening of the black cloud in her vision.
Let’s review just a few pearls of branch retinal artery occlusions. First, it is felt that BRAO’s comprise 38% of all acute retinal artery obstructions. They typically present with monocular vision loss and a relative visual field defect. Secondly, the fundus will have an area of whitening, possibly along the course of a branched arteriole as seen in this fundus photo from EyeRounds.org. Emboli are visible in the majority of cases, typically at vessel bifurcations. Typically BRAOs have a good visual prognosis, with vision improving to 20/40 or better in 80% of cases. The workup for BRAOs is similar to that of CRAOs, with carotid Doppler and cardiac echo to search for embolic sources. Finally, BRAOs can be seen in giant cell arteritis, so be sure to ask about GCA-risk factors, though BRAOs occur less commonly in GCA compared to CRAOs.